A hybrid model for clinical trials holds promise to save time, money, and lives
Testing new medicines with minimal site visits enhances safety during the pandemic. The same practice could lead to quicker, less costly clinical drug trials in times ahead.

Drug trials are expensive and cumbersome in normal times. Pharmaceutical companies spend, on average, $2.6 billion to develop a new drug and get it to market.1 And while results vary by discipline, only a fraction of drug candidates that enter clinical trials make it to market. The onset of the COVID-19 pandemic exacerbated this problem by interrupting drug trials and site visits. By April, the pandemic had disrupted hundreds of trials. By summer, that figure had grown into the thousands, according to GlobalData Healthcare.
The bulk of delays came from trials that suspended participant enrollment mainly due to patient safety concerns or a disruption in the clinical supply chain. However, the large number and furious pace of COVID-19-related clinical studies offer proof that researchers can run quicker and more flexible trials. Pharmaceutical executives frequently speak of innovation — taking new approaches to clinical drug trials — but often do not put innovation into action. The pandemic disrupted the traditional drug-testing paradigm. During this moment, researchers should try more actively to embrace an idea that’s already been considered for some time.
Shifting drug trials from a physical site-centric approach to a hybrid or decentralized model could lead to immediate and long-term benefits. In the near term, researchers can create a safer and more convenient process for study participants. In the long run, researchers can cultivate a more efficient and less costly method for testing new potential medicines. In both the short and long terms, a more decentralized approach will make it easier for participants to enroll and remain in studies that will lead to greater overall value for all stakeholders.
Decentralized, hybrid models will not change study designs. A hybrid model will simply make use of available digital technologies to enable more efficient and effective clinical processes. These improvements apply to recruitment, conduct, data management, safety monitoring, and patient engagement. Further, requiring fewer site visits holds the promise to expand test subject pools to look more like the real world.2
Testing new drugs for safety and effectiveness has not always been a billion-dollar enterprise. Tufts University’s Center for the Study of Drug Development found in 2013 that the all-in costs of new drug development had been increasing 8.5% faster than inflation.3 Increases in costs only heighten the pressure on companies to deliver new discoveries and replace fading revenue streams from older drugs.
Because of the spread of COVID-19, pharmaceutical companies have been unable to maintain continuity in studies and reach patients. The spread of COVID-19 obviously stalled many trials and delayed the development of many therapeutic treatments. As the pandemic persists, pharmaceutical companies must address a lingering set of problems:
- Diminished capacity for conducting trials.
- Smaller recruitment pools.
- Challenges keeping trial subjects engaged.
- Disruptions in supply chains.
Shifting the trial setting away from fixed sites can help address this by:
- Removing geographical constraints.
- Easing drug dosing (for certain protocols).
- Enabling richer telehealth.
That disruption appeared to be abating in some parts of the world in July — GlobalData statistics indicated a decline in the number of clinical trials disrupted. But trials in the U.S. continued to be disrupted at a high rate.4
Figure 1. Enrollment in drug testing has fallen dramatically in most specialties.
Source: Medidata, June 15, 2020
Regulators ready, investigators able
Industry regulators have laid out guidelines to allow for more flexibility while maintaining proper safety controls. The European Medicines Agency issued guidance this summer that accepts remote modes of site visits and safety monitoring and provides flexibility in critical sample collection and procedures, while retaining a priority on safety.5 Similar guidance from the U.S. Food and Drug Administration (FDA) suggests developing procedures for telephone – and video-based consent, remote site visits, and safety monitoring in consultation with internal review boards.6
In the past, a handful of established pharmaceutical companies including Pfizer, Eli Lilly, Sanofi, and Otsuka have explored decentralized or virtual trials. In 2011, Pfizer conducted a virtual trial for an overactive bladder drug candidate.7 Even earlier, Eli Lilly used 2004-vintage internet technologies to help manage a study on the effectiveness of an erectile dysfunction medicine.8 In the absence of a catalyst for change, researchers have not pushed further into decentralized testing.
Now that the pandemic drives renewed interest in decentralized drug trials, the technology available for investigators in 2020 has accelerated light-years away from the World Wide Web state of the art in 2004. In other industries, these technologies have become mainstream, and clinicians can rapidly adopt them for life sciences as regulators grow more flexible and investigators grow more familiar with them.
Shift from a physical site-centric approach to a virtual hub
In traditional drug trials, clinical sites serve as the hub for all trial processes. This “one-stop shop” provides value and convenience to the principal investigator, as all procedures, examinations, and data reside in that one location for all enrolled subjects at the site, usually in conjunction with a central site and oversight by a contract research organization.
A hybrid virtual hub model boasts of digitization and interoperable systems coupled with flexible governance and decision-making
Infosys has modeled ways to shift from physical sites to a virtual hub, in which researchers execute and manage the same clinical study processes but without geographic constrictions. The goal is to remove current constraints on potential study subjects and execute trials more efficiently. A hybrid virtual hub model employs digitization, interoperable systems, and a flexible approach to governance and decision-making.
To construct a decentralized or hybrid drug trial, researchers should:
Integrate digital capabilities across clinical development locales and nodes. This will free trial processes from a physical site.
Build a virtual trial platform using interchangeable modules. This gives researchers the ability to use plug-and-play capabilities such as electronic consent, patient monitoring, and specific direct data capture tools that address the particular needs of a clinical trial or patient location.
Develop a culture of communication and embrace change throughout the effort. This will increase flexibility during trials. Take a vendor-agnostic approach. This will allow clinicians to integrate the best capabilities regardless of providers or platform. Use real-life business experiences to design and execute trial processes. Explain real-life business experience and its benefits.
Virtual health care provides a tailwind for hybrid trials
Health care providers are investing heavily in telemedicine infrastructure and benefiting from higher reimbursement from payers. Virtual care delivery was growing fast before COVID-19 and now has been thrown into overdrive.9 With some 50%-70% of primary care visits conducted virtually, it’s a perfect opportunity to integrate clinical study visits with virtual care delivery models.10
Hybrid or decentralized trial design eliminates geographic constraints for clinical trials and expands access to clinical trials for patients. As there are more than 6,000 rare conditions, shifting from the central site holds special promise for trials focused on rare diseases.
In 2018, Genentech used a hybrid site-based and virtual model to recruit participants for phase 3 trials of a treatment for a rare autoimmune disease. In taking the hybrid approach, investigators found virtual recruitment was much faster than traditional methods.11 Subsequently, the drug Rituxan (rituximab) became the first FDA-approved treatment for pemphigus vulgaris, which causes severe (and unsightly) skin and mouth blisters.
How to make hybrid models stick
Drug candidates that make it through phase 3 very often achieve FDA approval. This is a credit to the traditional centralized process. As researchers experiment with hybrid and decentralized trials, they should remain aware that there is much to learn from the traditional experience. Further, adjacent industries also can offer ideas that can be reframed for life sciences.
In traditional site-centric trials, participants who interact with lead physicians remain more engaged in the study. For hybrid and decentralized contexts, investigators should consider applying digital marketing tactics proven to work in consumer models. Key aspects of online recruitment for trials include:
- Analyze data to identify prospective participants.
- Attract subjects using relevant content.
- Lock in participants by devising instant or near-instant decisions.
- Use doctor interaction and interviews to sustain engagement in the study.
- Demonstrate a commitment to privacy that reassures the patient and reinforces compliance and ethical standards.
Biopharma can learn from the strategies pursued by consumer-focused enterprises to improve recruiting for drug trials. Tactics include learning to find the right target audience, employing multichannel marketing strategies and leveraging commercial customer platforms to build recruiting channels.
The path away from site-centric trials
Shifting to a hybrid approach to drug trials requires an assessment of which activities can be shifted closer to the participants. That does not necessarily mean making a technology-aided leap from central clinical site to virtual visit. It could mean shifting from that central site to a local clinic or making a home visit to the participant.
To assess how far an activity can be shifted, study designers first must consider patient safety and then the complexity of the infrastructure or equipment it requires:
- Identify activity.
- Assess safety.
- Measure infrastructure and equipment complexity.
- Ensure data quality.
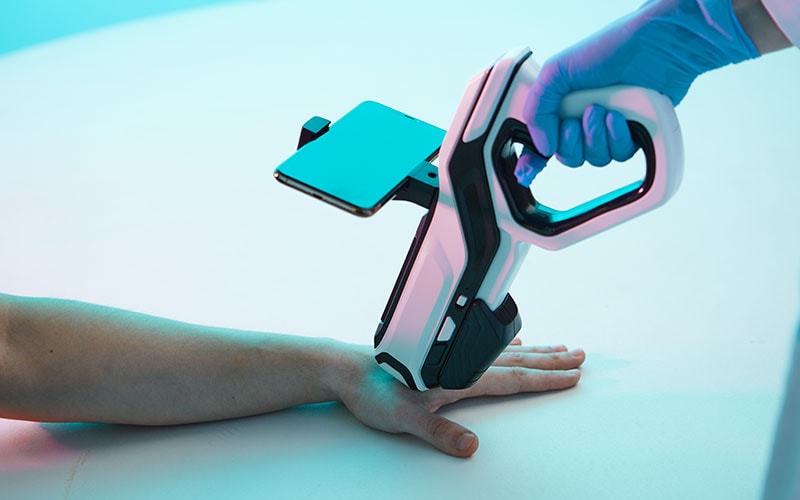
Site visits provide high-fidelity data that researchers can trace and audit using electronic medical records. Off-site, wearable, and connected devices can provide timely and accurate patient data with the appropriate level of traceability and authenticity required for clinical trials . Direct data capture using devices and sensors cuts down on the frequency of site visits and reduces time needed to capture data. That said, the variety of devices and variations in their data could present some challenges, but a systematic approach can handle those challenges by following these principles:
- Codify the source of data points by device and location.
- Identify acceptable variability and impact on trial design.
- Identify devices that work within that variability and are readily available to participants.
- Validate data quality from identified devices.
- Create incentives and rewards for participants to deliver data on time and in good order.
- Apply artificial intelligence (AI) and machine learning to benchmark device data. This has value for the current trial and as a knowledge base for future trials.

Off-site, wearable, and connected devices help with accurate and timely patient data while providing traceability and authenticity
In decentralized trials, study participants will play an increased role in capturing data. This information must be held to the same standard as in traditional clinical studies. Telemedicine and electronic medical record updates can be another route to capture this data.
Figure 2. A hybrid approach to drug trials shifts activities closer to participants when it is safe and simple.
Source: Infosys
In a typical site visit, a patient may have his or her heart rate checked once. Some wearable devices can deliver heart rate data second by second.12 (That’s 86,400 measurements in a day per patient.) Managing such a volume of data will require cloud-based streaming technology and real-time analytics to distill meaningful data. Cloud-based streaming technology can lead to trial-specific analytical models. Developing these models in a compliant environment will be a critical overhaul required to support virtual trial models.
Data monitoring teams with the ability to detect abnormal data and communicate with patients can help keep the volumes of data clean. These teams can use AI and machine learning to help with the monitoring and to pick up indications of problems in terms of data quality or patient safety early on.
Generally, the most important data in clinical trials comes from samples studied in laboratories. Traditional models require physical site visits and qualified technicians to collect blood, tissue, or other bio samples. Sample collection for trials in hybrid models requires technology-enabled supply chain support with home-based sample collection or a nearby sample collection center. Such systems are already in practice outside the laboratory. U.S. regulators currently have approved three distinct types of at-home colon cancer screening tests in which patients collect their own samples.13 Sample containers can be shipped to these nearby locations, with virtual collaboration channels to support sample collection protocols.
Clinical sites serve as the nerve center for traditional trial processes. In a decentralized model, these processes can be shifted to patients and third parties such as home-based medical services enterprises. Orchestrating the activities of participants, researchers, and service providers will require technical integration and precision. Research organizations can look to other industries (e.g., multichannel retailers) for frameworks and guidance. Imagine an integrated system with links to mobile devices that enables anytime-anywhere collaboration and delivers an Amazon-like patient experience.
This transition requires reimagining trial design with a virtual-first mindset and establishing a robust technology foundation. Decentralized trials hold the promise to accelerate the journey to better drug development — benefiting patients and pharma companies alike.
References
- Innovation in the pharmaceutical industry: New estimates of R&D costs, Joseph A. DiMasi, Henry G. Grabowski, Ronald W. Hansen, Journal of Health Economics, May 2016.
- Diversity in clinical trials defines good science and better medicine, Jane L. Delgado, Edward Abrahams, STAT, January 17, 2019.
- Innovation in the pharmaceutical industry: New estimates of R&D costs, Joseph A. DiMasi, Henry G. Grabowski, Ronald W. Hansen, Journal of Health Economics, May 2016.
- Clinical trial disruption due to Covid-19 has begun to decline, GlobalData Healthcare, July 9, 2020.
- Guidance for medicine developers and companies on COVID-19, European Medicines Agency, accessed June 23, 2020.
- FDA Guidance on Conduct of Clinical Trials of Medical Products during COVID-19 Public Health Emergency, U.S. Food and Drug Administration, June 3, 2020.
- Pfizer conducts first “virtual” clinical trial allowing patients to participate regardless of geography, Kristen Neese, Pfizer Inc., June 7, 2011.
- From Informed Consent through Database Lock: An Interactive Clinical Trial Conducted Using the Internet, Kristin L. Ellenberg, Amy M. Hoover, Michael L. Rutherford, Drug Information Journal, July 1, 2004.
- Being Resilient: Progressing from Telehealth to Digital Care, Venky Ananth, Manojit Sarkar, Chad Watt, Infosys Knowledge Institute, July 2020.
- COVID-19 Pandemic: The Surprise Catalyst for Telemedicine Adoption, Healthcare Growth Partners, HIT Consultant, May 8, 2020.
- Industry embraces the virtual trial platforms, Caterina Lucchini, Pharmaworld Magazine, June 4, 2018.
- Understanding continual (24/7) optical HR data and resting heart rate, Ray Maker, DC Rainmaker, Feb. 16, 2016.
- Just do it… yourself: At-home colorectal cancer screening, James Richter, Harvard Medical School Health Blog, March 12, 2019.







